In today’s competitive behavioral healthcare landscape, knowing how to get hospital referrals for mental health services can be a game-changer for growth. Hospital referrals not only help generate new clients but also ensure continuity of care for patients in need. However, securing these referrals requires strategy, relationship-building, and a sense of urgency.
At Supportable, not only do we work with dozens of behavioral health providers facing this exact challenge, our team members have managed practices ourselves and experienced it first-hand.
We’ll cover how to build trust with hospital staff, meet necessary credentials, improve communication, overcome common barriers, and leverage technology (like behavioral health software and a patient CRM) to stand out and scale up your practice.
1. Build Strong Relationships with Hospital Staff
When it comes to getting referrals from hospitals, relationships are everything. Hospital discharge planners, social workers, and psychiatric unit coordinators are often the gatekeepers who decide where patients go next. Establishing trust and familiarity with these key players is the first step in securing a steady stream of referrals. Here’s how to cultivate those crucial connections:
Initiate Contact with Empathy and Clarity
Don’t wait for hospitals to find you – reach out and introduce your facility. A friendly phone call or an email to a discharge planner or social worker can open the door. Explain who you are, the services you provide, and why you’re reaching out. For example, you might say something like,
We understand how critical timely follow-up is after discharge. Our clinic can schedule your patients for a therapy session within 48 hours of release, ensuring they don’t slip through the cracks.
Show that you share the hospital’s goal of quality post-discharge care. Be clear, professional, and above all, empathetic in your tone. Acknowledge the challenges hospital staff face and position your facility as a helpful partner ready to alleviate some of their burden.
Provide Helpful Leave-Behind Materials
 Whenever you meet or visit hospital teams, come prepared with a small arsenal of marketing materials. Bring brochures and business cards for your practice, and leave them in the hands of discharge planners or in common areas of psychiatric units. Don’t be shy! This is common practice. These tangible reminders keep your name on their radar. Make sure your brochures succinctly highlight your services, unique approaches, and success stories.
Whenever you meet or visit hospital teams, come prepared with a small arsenal of marketing materials. Bring brochures and business cards for your practice, and leave them in the hands of discharge planners or in common areas of psychiatric units. Don’t be shy! This is common practice. These tangible reminders keep your name on their radar. Make sure your brochures succinctly highlight your services, unique approaches, and success stories.
A one-page “referral guide” or checklist outlining how to refer a patient to you can also make the hospital staff’s job easier. By leaving behind an informative brochure and a stack of cards, you’re providing hospital personnel with quick reference tools and making it effortless for them to point patients your way.
Schedule Regular Check-Ins and Collaborative Meetings
Building a relationship isn’t a one-and- done deal. Set up regular meetings or check-in calls with hospital discharge planners and social workers to discuss patient needs, refine the referral process, and address any hiccups. For instance, you might arrange a monthly coffee or a quick Zoom meeting with the key contact at each hospital unit. Use these conversations to ask how referred patients are faring, what feedback the hospital has, and how you can improve the process. This level of ongoing collaboration not only keeps everyone on the same page, but also demonstrates your commitment. Over time, these check-ins build trust and a sense of partnership.
Hospitals want to see that you’re not just interested in getting referrals, but also in managing them well and ensuring their patients are cared for. In a competitive environment, being consistently present (without being pushy) helps you stand out from other facilities vying for attention . Remember, hospital staff are incredibly busy (you know, saving lives and all!). By proactively maintaining the connection, you make their life easier and your facility the first they’ll think of when a patient needs aftercare.
Offer Value through Education and Support
One way to solidify your partnership is by providing value-added services to the hospital. Consider offering educational workshops or in-service training sessions for hospital staff. For example, you might host a short lunch-and-learn about effective approaches to substance use aftercare, or updates on the latest mental health treatment modalities your clinic offers.
This kind of information can deepen hospital staff’s understanding of how your facility can help their patients. It also positions you as an expert resource rather than just another vendor. Keep these sessions practical and respectful of staff time – perhaps a 20-minute presentation plus Q&A.
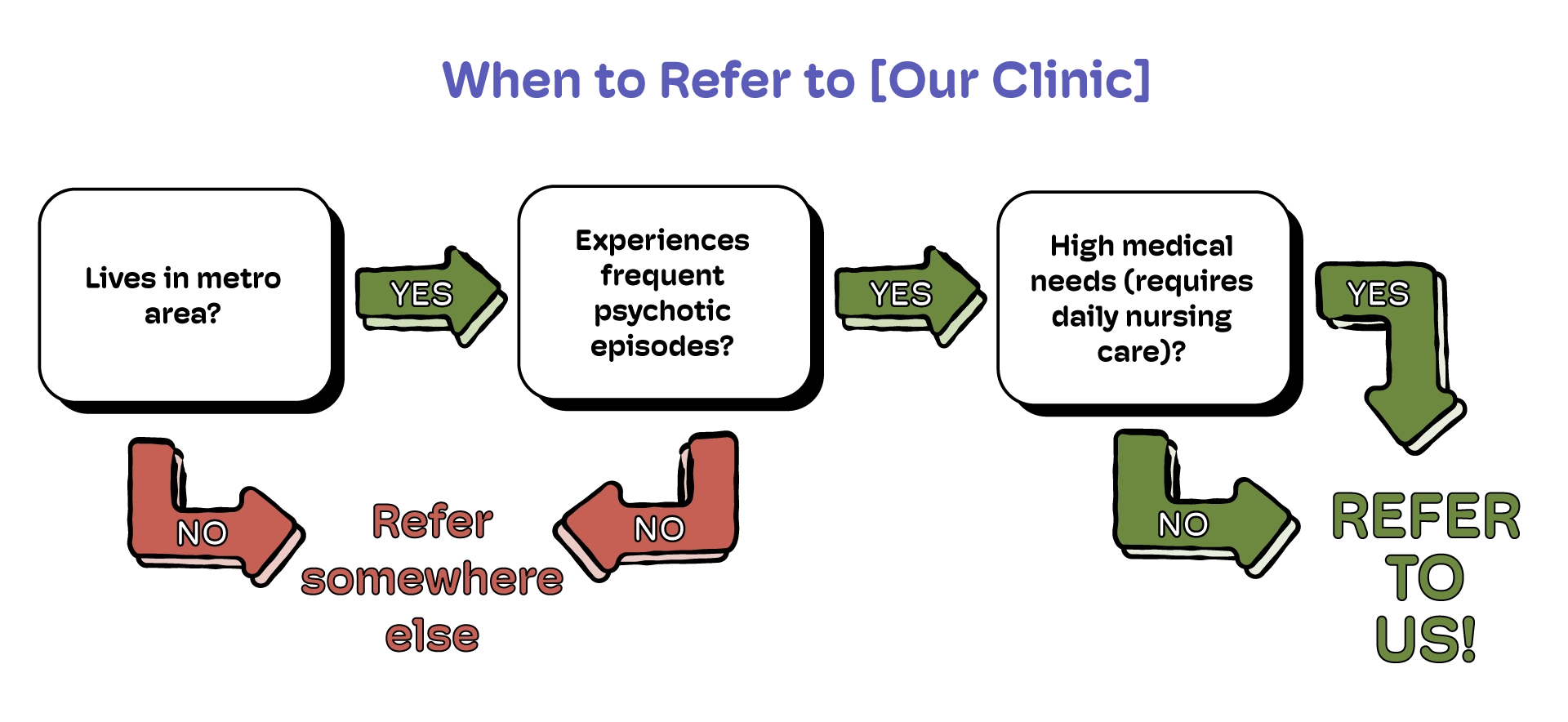
By educating hospital teams about your services and how to navigate the referral process with you, you foster stronger relationships and mutual trust. You might even provide quick reference handouts during these sessions (e.g. a flowchart of “When to refer to [Your Clinic]”).
The more comfortable and knowledgeable hospital staff are about your organization, the more likely they’ll refer patients. Mutual benefit is key: show them how referring to you makes their job easier (and their patients’ outcomes better), and they’ll be more inclined to pick up the phone and call you next time.
Practical Tip: Always leave each meeting with a clear next step.
For example, offer to send a follow-up email recapping any decisions or to provide extra brochures if they run low. This makes follow-up easier and keeps the momentum going. Before you part ways, you might say, “I’ll email you that referral form template we discussed so you have it on file,” or “Let’s touch base next month to review how the last few referrals went.” By setting a follow-up expectation, you take the onus off the hospital staff to remember – your proactive approach will be appreciated.
2. Ensure Proper Credentials and Formal Agreements
Building great relationships will get you far, but hospitals also need to know that your facility meets all requirements and that referrals will be handled seamlessly. In this industry, credibility and compliance are non-negotiable. To instill confidence and avoid any administrative roadblocks, make sure you cover these bases:
Meet Credentialing Requirements and Standards
Ensure your practice and staff have all necessary licenses, certifications, and credentials required to accept referrals from hospitals. Hospitals often have vetting processes for external partners. This might include your clinicians’ licenses, any accreditations for your facility, proof of insurance, etc. Being fully credentialed and in compliance with regulatory standards (state, federal, and industry-specific) means there’s no hesitation when it comes time to refer a patient.
If you specialize in certain treatments (e.g. substance use disorder programs or adult foster care services), highlight any special certifications or program licenses you have. Having these ducks in a row demonstrates professionalism. It signals to the hospital, “We take quality and safety as seriously as you do.”
Establish Formal Referral Agreements
While a handshake and goodwill go a long way, a formal written agreement can cement the partnership. Work with the hospital (likely their administration or legal department) to create a written referral agreement or Memorandum of Understanding (MOU). This document should outline how the referral process will work step by step: for example, how information will be exchanged, expectations for admission timelines, responsibilities on both sides, and any reporting or feedback loop. Formal agreements provide clarity and accountability for both parties. They set the tone that you are committed to a reliable process.
Not every hospital will require a contract, but being open to one – or even suggesting it – shows a high level of seriousness. It also gives you a chance to explicitly address important details like patient consent handling and data sharing protocols (more on that soon). In short, having an agreement in writing can prevent misunderstandings down the line. If a hospital has a preferred provider network or approved list, aim to get your facility listed. That often involves paperwork and proving credentials, but once you’re an official “preferred referral partner,” you’ve cleared a huge hurdle in getting consistent referrals.
3. Streamline Communication and Follow-up
Even after you’ve established a connection and set up an agreement, the day-to-day mechanics of referrals can make or break the partnership. Hospitals will favor partners who make the referral process easy, transparent, and responsive. It’s up to you to streamline communication and stay on top of follow-ups so that hospital staff feel confident their patients are in good hands. Here are some best practices:
Create a Clear, Simple Referral Process
If you want more referrals, make referring to you as easy as possible for hospital staff. This means providing clear instructions and having a streamlined process. Develop a standardized referral form that outlines exactly what information you need (patient info, discharge summary, insurance details, etc.) and how they should send it to you. Ensure your contact information (phone and email for your intake coordinator or on-call staff) is prominent and up to date. Some hospitals might have their own referral system – adapt to it if you have no choice, but still clarify your needs.
The idea is to remove any guesswork. If a social worker has to hunt around for how to refer to your clinic, you might lose that referral. Consider creating a dedicated referral packet that you can give to hospital teams: it might include brochures and even a FAQ for common questions. Some people even leave a tablet on the unit on a stand with a link to their referral form, solely to be used to send referrals directly to their business. By standardizing and simplifying the referral pathway, you show respect for the hospital staff’s time and make it more likely they’ll use your pathway repeatedly.
Follow Up Fast (and Keep Following Up)
Once a hospital refers a patient to you, your responsiveness is on trial. Aim to follow up promptly with both the hospital and the patient. For example, if you receive a referral in the afternoon, try to contact the patient that same day or by the next morning to start the intake process. At the same time, shoot a quick update to the referring person (if appropriate under privacy guidelines) – e.g., “We’ve received your referral for John D., thank you. We have contacted him and scheduled an intake for Friday.” This closes the loop and gives the hospital peace of mind that the patient is not falling through.
Also, keep the hospital in the loop on major developments, within the bounds of consent – for instance, let them know when the patient is admitted to your program or inform them of initial treatment plans if they desire feedback. Many referring providers appreciate hearing that their patient actually got the help they needed. Being diligent in follow-up sets you apart because, sadly, lack of follow-through is a common pitfall. A large percentage of referred patients never make it to the next provider due to poor follow-up coordination. Don’t let a referral be yet another dropped ball.
Be Polite, Persistent, and Organized
Communication with hospital partners should be consistent without becoming a nuisance. Strike a balance: you don’t want to spam your contacts with daily calls, but you also don’t want to disappear on them. One approach is to set a routine for follow-ups – for example, after a patient is referred and admitted, send a brief update to the hospital team within 24-48 hours, then perhaps a summary of the patient’s status after a couple of weeks (if appropriate and agreed upon). Always secure patient consent for information sharing, of course.
If a hospital hasn’t sent any referrals in a while, a polite check-in email to ask if there have been suitable cases, or to simply share a success story or new program at your facility, can rekindle the connection. The key is to stay front-of-mind in a helpful way. And if a hospital staff member reaches out with a question or request, prioritize that response. Rapid, attentive communication makes you look reliable and easy to work with – exactly what hospitals want in a referral partner.
Leverage Technology for Faster Transfer of Information
The days of faxing paperwork back and forth are fading. While fax is widely known, legendary even, for being HIPAA compliant, it’s still painfully analog in today’s fast-paced world. There are a number of interesting AI solutions in the pipeline to process faxes, so now is a perfect time to embrace technology to smooth out communication.
All that said, Consider using a patient CRM or referral management software (more on this later) that allows you to track referral status and automatically notify hospital partners of key events. Technology not only saves time but also reduces errors (no more lost faxes or misdialed phone numbers). It shows the hospital that your operations are modern and efficient. Just be sure any tech you use is HIPAA-compliant and that both sides are comfortable with it.
A well-implemented tech solution can turn what used to be a cumbersome process into a quick, secure, and transparent workflow – a win-win for both you and the hospital.
4. Overcome Common Barriers to Referrals
Even with strong relationships and smooth processes, you’ll inevitably face challenges when coordinating referrals from hospitals. Being prepared to address these common barriers will help you keep the referral pathway open and effective. Here are a few hurdles that often come up – and how to tackle them:
Bed Shortages or Capacity Limits
One frequent frustration is when a hospital wants to refer a patient, but your facility has no open beds or appointment In a high-demand environment, this can happen, but how you handle it makes the difference.
Maintain a real-time inventory of your availability and communicate it proactively to your hospital partners . For example, if you know you’re running at capacity this week, give the discharge planner a heads-up so they aren’t caught off guard. It may feel counterintuitive to advertise when you’re full, but transparency builds trust. Also, develop a contingency plan: if you can’t take a patient immediately, can you refer them to a trusted partner facility (and maybe have an understanding that they’ll do the same for you)?
Creating a small network of allied facilities can ensure patients still get placed quickly even if it’s not with you. Hospitals will remember that you helped find a solution rather than just saying “sorry, can’t help.” Additionally, continually evaluate your capacity management – if you’re frequently turning away referrals due to bed shortages, that might be a sign to expand your capacity or optimize your intake flow (perhaps using technology or better scheduling to increase throughput). The more patients you can accommodate in a timely manner, the more valuable you are to hospitals.
Patient Consent and Information Sharing
Privacy laws (like HIPAA in the U.S.) and ethics require that patients consent to have their information shared between providers. Sometimes, referrals get stuck because a patient hasn’t agreed to share their records or is uneasy about transferring care.
To overcome this, build a consent process into your referral workflow from the start. Work with hospital staff to ensure the patient is informed about the referral and signs any needed release forms before leaving the hospital. It helps to provide patients (and hospital staff) with a clear explanation of why the referral is recommended and how it benefits the patient. For instance, a patient might fear they’re being “passed off” – both you and the hospital can reassure them that this is about getting specialized care, not abandonment.
Insurance and Payment Hurdles
Another common barrier is the financial and insurance aspect of care. The Big Beautiful Bill will make it even more challenging as individuals lose their coverage. Perhaps the patient’s insurance isn’t in-network with your facility, or their coverage for mental health services is limited. Hospitals often have social workers or financial counselors who try to place patients in programs their insurance will cover – you’ll need to collaborate with them.
Be upfront about which insurance plans you accept, and if possible, consider expanding your network participation if you notice many referrals are being impeded by insurance mismatches. For cases where coverage is a problem, work closely with the hospital’s team to explore solutions.
Can the patient be eligible for any state or charity programs?
Do you offer sliding scale fees or payment plans for self-pay patients?
Sometimes a hospital may have funds for complex discharge planning that could assist with a short-term placement. Showing that you’re willing to get creative to help the patient goes a long way. It may not always result in a referral you can take (some cases just won’t be financially feasible), but your collaborative spirit will be remembered.
Ultimately, the easier you make it to handle the financial side, the more referrals will successfully convert to admissions instead of falling apart due to insurance snags. A good behavioral health software can also handle real-time eligibility verification to get you the information you need immediately (more on this later).
5. Leverage Behavioral Health Software and Patient CRM Tools
One major way to elevate your referral game (and impress your hospital partners) is to use technology to your advantage. Modern behavioral health software solutions, particularly a dedicated patient CRM (Customer Relationship Management) system, can streamline your referral and intake process tremendously. Not only do these tools make your operations more efficient, but they also signal to hospitals that you run a tight, data-driven ship. Here’s how leveraging the right software can transform your referral pipeline:
Streamline Referral Tracking and Management
A healthcare-specific CRM or referral management system lets you keep track of every referral in one centralized dashboard. No more sticky notes or messy spreadsheets – you can see at a glance which patients were referred, their status (contacted, scheduled, admitted, etc.), and any tasks pending.
This level of organization means you’ll never drop the ball on a referral. It also allows multiple team members to coordinate (for example, your intake coordinator and a billing specialist can share notes on a referral while staying in their respective lane).
By efficiently managing referrals, you ensure patients don’t fall through the cracks and that hospitals feel confident sending people your way. If a hospital ever wants an update, you can provide it promptly because all information is at your fingertips.
Integration with Existing Systems
The best behavioral health software won’t exist in a vacuum – ideally, it integrates with your existing EHR and can interface with hospital systems. For example, Supportable (a HIPAA-compliant Behavioral Health CRM we’ll discuss more in a moment) is designed to flexibly integrate with various electronic health record systems.
This means information can flow securely between the hospital and your clinic without redundant data entry. When you show a hospital that you can exchange referrals and updates electronically (maybe even directly from their system to yours), it removes a lot of friction. Integration leads to faster admissions and less paperwork. It also positions your facility as tech-forward and adaptable. Even if you can’t have full integration with a hospital’s system, being able to process information digitally is a game changer.
In short, your tech should play nice with others. When it does, everyone benefits: the referral is processed faster, the patient’s info is accurately transferred, and your staff spend less time copying data from fax sheets.
Gain Insights with Data Analytics
Another powerful aspect of using a CRM or similar software is the ability to analyze your referral data. Over time, you can gather insights like:
Which hospitals or units send you the most referrals?
What types of cases have the highest conversion to admissions?
Where do bottlenecks occur in your intake process?
By reviewing these patterns, you can make informed tweaks to your strategy. For example, if data shows Hospital A’s referrals often stall at the insurance verification stage, you might proactively work with that hospital to streamline pre- authorization. Or you might discover that referrals from Hospital B have a 90% show-up rate for intake, whereas another source is much lower – prompting you to focus your relationship-building efforts on the high-yield source.
Data can also help demonstrate your value to hospitals: imagine being able to report,
“In the last quarter, of the 20 patients you referred to us, 18 were admitted within 5 days and 0 were readmitted to the hospital within 30 days.”
Those are powerful metrics that make your case as a worthy partner. In essence, a good system doesn’t just collect data, it helps you use data to continuously improve and prove the effectiveness of your referral pathways.
How to Get Hospital Referrals for Mental Health More Easily With Supportable
Here’s where we come in. Supportable – a HIPAA-compliant Behavioral Health CRM specifically designed for mental health and substance use treatment providers.
Supportable provides a unique referral management experience tailored to intake workflows. What does that mean for you? In practical terms, Supportable can integrate with your existing EHR (so it complements, not complicates, your current tools) and serve as the command center for all your referrals. It helps streamline the referral process from start to finish: logging a new referral, guiding your staff through each intake step, and even automating communications like sending appointment reminders or follow-up emails to the referring hospital.
By using a tool like Supportable, you can significantly reduce the time it takes to get patients into care – which hospitals love to see, because it means patients aren’t languishing after discharge.
Supportable also leverages data analytics (as discussed above) to pinpoint your most effective referral sources and highlight areas to improve. For example, it might show that referrals from Hospital X have a much faster conversion when a particular staff member handles them – indicating a best practice to replicate, or it might identify that patients coming from Hospital Y tend to need a certain program, informing you to perhaps expand that service. These insights ultimately help you optimize your intake process and allocate your marketing or outreach efforts wisely.
Perhaps most importantly, using Supportable can help your facility stand out in the eyes of both hospitals and competitors. Hospitals will notice that you have a professional system in place – they’ll experience seamless communication, timely updates, and well-organized coordination.
Meanwhile, many of your competitors might still be juggling phone calls and sticky notes, missing follow-ups, and presenting a disorganized front.
By investing in technology, you signal that your practice is operating at a higher standard. This not only impresses referral sources but also positions you to scale up your operations. With efficient software handling the heavy lifting of tracking and communications, your team can manage a larger volume of referrals and clients without feeling overwhelmed. In other words, tools like Supportable enable you to grow your client base (and revenue) sustainably, while maintaining quality care.
(Empathy note: We know implementing new software can feel daunting – there’s a learning curve and a cost. But consider the cost of not having it: missed referrals, slower growth, and getting outpaced by tech-savvy competitors. Even a modest patient CRM can pay for itself by helping you capture just a few referrals that might have otherwise slipped away.)
Conclusion: Stand Out, Scale Up, and Serve More Clients
Establishing effective referral pathways from hospitals is one of the most direct ways to generate new clients for your behavioral health practice while also ensuring patients receive the timely care they need. It’s a win-win scenario: hospitals achieve better outcomes and smoother discharges, and your clinic gains a steady stream of clients who genuinely need your help. But as we’ve discussed, winning these referrals requires a proactive and polished approach. You need to build genuine relationships, communicate relentlessly (yet tactfully), and remove any barrier that might hinder a referral from turning into an admission.
The behavioral health field is competitive – other clinics and programs are likely knocking on the same hospital doors. By following the strategies outlined here, you can rise above the noise. Be the partner who is reliable, responsive, and easy to work with, and your reputation will grow. Remember to infuse empathy into every interaction; hospitals will see that you truly care about their patients’ well-being, not just your intake numbers. And don’t be afraid to inject a bit of personality – a friendly, human touch (and occasionally a sense of humor) can make you more approachable and memorable to busy healthcare professionals.
Remember: effective referral pathways are not just about business growth – they’re about ensuring patients seamlessly transition to the care that can change their lives. With the right relationships and tools in place, you can make that transition smoother for everyone involved. Good luck, and go make those connections!

